COVID 19: Projections and Conjectures
This essay explores some of the strategies being used to mitigate, contain, and eliminate the threat of the COVID 19 virus. My interest is primarily the global impact, but I have used local data --specifically Ontario data-- to illustrate the effectiveness of the strategies being used to i) lessen the mortality rate of the virus, and ii) eliminate the threat posed by the virus. I make a sharp distinction between these two, often conflicting objectives, their limitations, and how the pursuit of these objectives is playing out in the world.. I will begin with the "flattening of the curve" objective, followed by the "elimination of the threat" objective, and go on to explore how these two objectives may be at odds with each other, and some of the implications of that both locally and globally. I draw some tentative conclusions from my analysis, and end by posing unanswered questions about the impact of COVID 19 on the world.
The objective of “flattening the curve” is to reduce the spread to numbers that will not overwhelm healthcare systems. That means that the available healthcare resources are enough to identify and meet the needs of those who have been infected and are consequentially in need of healthcare services. Most of those who have been infected will recover without medical intervention (about 97%). It is the vulnerable populations –the elderly, those with compromised immune systems, those who have preexisting medical conditions, those whose employment and/or social conditions don't allow for self-isolation, etc.--that may need medical intervention if they become infected.
The capacity of the
healthcare system to provide care for critically ill patients is
limited by: available infrastructure like hospital beds and ICU beds;
the number of ventilators; the number of trained medical
professionals; available cleaning, maintenance and administrative staff; and access to the personal protection equipment (PPE) needed to protect all
personnel from infection. If the numbers of vulnerable people
infected exceeds any of these capabilities to safely treat infected
patients, many COVID 19 positive patients will die.
 | ||||||
| The capacity of the healthcare system is exceeded when the number of COVID 19 cases rises above the red line. Herd immunity is reached only after the number of recovered COVID 19 cases (people who have developed antibodies) rises above the green line. |
There are three primary ways
of reducing the burden on the healthcare system. One is to identify
and isolate/quarantine all carriers of the virus –testing. The second is reducing opportunities for people
--both those who have tested positive and all those who may be positive
but not yet been tested-- from passing on the virus to others --physical distancing. The
third is to identify the most vulnerable populations and take
additional steps to ensure that they don't come in contact with
anyone who has been infected --making sure seniors and long term care homes residents and staff, shelters, prisons, etc. are isolated from the virus --a sort of inverse quarantine.
Testing:
The
numbers of available tests, personnel, and PPEs to safely carry out
tests is increasing, so more people are now being tested. While more
testing is increasing the number of confirmed positive cases, knowing
who
is a carrier, even if they are asymptomatic, is very beneficial.
Testing helps identify additional carriers by tracing the movements
of positive patients back to likely source carriers (tracing) so that sources too
can be identified, isolated/quarantined, and treated if
necessary.
Testing capacity, although increasing, remains limited, so
not everyone is being tested. Those prioritized for testing are
primarily members of vulnerable populations, and the medical personnel and personal care workers who look after them. Those who are otherwise exposed to large numbers of
people in the course of their “essential employment", and/or who
live in overcrowded or otherwise adverse social conditions, may also
get higher priority for testing than others. Those who aren't members of
vulnerable populations, aren't essential workers, and aren't
displaying symptoms remain a low priority, and are simply being asked
to stay at home, wash their hands, sneeze into their elbows, and
avoid all unnecessary contact with other people.
Physical
Distancing:
Physical distancing is not about preventing
the
spread, but rather reducing the
rate
of
the spread. The virus cannot spread very quickly if the opportunities
for transmission aren't there. (see Herd Immunity diagram below.) Physical distancing reduces these
opportunities, which will help flatten the curve. Flattening the curve will help
reduce the burden on the healthcare system at any given time. Social
distancing won't ensure that people are never
exposed to the virus; it can only buy time, so that future
transmissions occur some time after those currently in acute care have either
recovered or died, thereby freeing up beds and other healthcare
resources necessary to accommodate new cases.
Identifying and Protecting the Most Vulnerable Populations: Identifying and protecting the most vulnerable populations is also very important, because it is these people who, if they contract the virus, are most likely to need a lot of healthcare resources. We already know that the elderly and those with suppressed immune systems and other preexisting medical conditions are among the most vulnerable. Healthcare and personal care workers must take special care to ensure that they don't contract, or, as importantly, transmit the virus to their patients or each other. In addition to hospitals another large proportion of the vulnerable are living in institutions for long-term care, so steps must be taken to ensure that staff working in these institutions are not introducing the virus into these vulnerable populations. Some care providers work in two or more institutions. These must take special care that they are not inadvertently cross-contaminating one institution with a virus they may have contracted in another. Because staff are often underpaid and only offered part-time work with no benefits, many are financially obligated to take on two or three jobs in similar institutions, thus increasing the risk of cross-contamination.
Identifying and Protecting the Most Vulnerable Populations: Identifying and protecting the most vulnerable populations is also very important, because it is these people who, if they contract the virus, are most likely to need a lot of healthcare resources. We already know that the elderly and those with suppressed immune systems and other preexisting medical conditions are among the most vulnerable. Healthcare and personal care workers must take special care to ensure that they don't contract, or, as importantly, transmit the virus to their patients or each other. In addition to hospitals another large proportion of the vulnerable are living in institutions for long-term care, so steps must be taken to ensure that staff working in these institutions are not introducing the virus into these vulnerable populations. Some care providers work in two or more institutions. These must take special care that they are not inadvertently cross-contaminating one institution with a virus they may have contracted in another. Because staff are often underpaid and only offered part-time work with no benefits, many are financially obligated to take on two or three jobs in similar institutions, thus increasing the risk of cross-contamination.
Those
living and/or working in shelters, prisons, reservations, refugee
camps, on the streets, or any other over-crowded and/or less-than-sanitary
conditions are also more vulnerable. Social distancing, hand-washing,
etc. are very difficult, if not impossible, in such social
conditions. Also, for those whose 'home' is a small room somewhere,
which may or may not have cooking facilities, or may require sharing
a bathroom, or not allow for the option of working from home, cannot
maintain the same level of social distancing that more affluent
citizens can. When it comes to vulnerability, class is very much an
issue. It is no longer only those who can afford to take a cruise on
a cruise ship, or winter in Florida, who are contracting the virus. The
latter may be primarily responsible for bringing the virus into the
country, but at this point there are as many, if not more community-based sources of infections as there are traveller-based sources. Everyone
is at risk, and the most fertile ground for spreading the virus is on the very bottom rung of
the socioeconomic ladder.
Herd Immunity --Eliminating the Threat of Infection:
In the measures described above the goals were i) reducing the rate of the spread to numbers the healthcare system can safely handle, and ii) increasing the ability of the healthcare system to provide care for all those in need of it --more ventilators, PPEs, tests, etc. These measures will neither exterminate the virus, nor eliminate the threat. The only people currently not at risk are those who have already been infected and recovered –those who have built up a sufficient supply of antibodies to fight off any future exposure to the virus. But for how long will we continue to be at risk? For however long it takes the community of people we interact with to develop what is called “herd immunity”.
Herd
Immunity
 |
| The bottom two quadrants depict herd immunity. |
The
risk of infection will remain until we have developed what is called
“herd immunity”. Herd immunity is reached in one of two ways (or
a combination of both): The first way is a vaccine. People who have
been vaccinated against a virus generate antibodies that both protect
them from becoming ill due to exposure, and prevent them from
becoming carriers –from transmitting the virus to others. The
second way of developing herd immunity will come about naturally when
enough of the population has become infected and recovered from the
COVID 19 virus. Like people who have been vaccinated, recovered
people will have developed antibodies that both protect them from becoming
ill due to new exposures, and unable to carry enough of the virus to
allow for transmission to others.
Coronavirus:
Are we getting closer to a vaccine or drug?
Tests
like these are taking place much quicker than would normally be the
case, and some are using new approaches to vaccines. ...But
even if these -or any other tests- do prove successful, it's not
expected that manufacturers will be able to produce a mass-produced
vaccine until the second half of 2021.
Herd Immunity reached Through Infection and Recovery: Without a vaccine herd immunity will only be reached when enough people have been infected and recovered from COVID 19. Presumably these people will have built up enough antibodies to protect themselves from becoming ill a second time, and to prevent them from being carriers --from spreading the virus to others who have not yet been exposed. I say 'presumably' because there is much that is still unknown. For instance, it is unknown whether or not the antibodies these recovered people develop will last indefinitely, or will need to be replenished by repeated exposures to the virus. Without a vaccine there can be no booster shots. It is also unknown whether or not their antibodies will be able to fight off mutations of the original virus. The virus will undoubtedly mutate, but so far it looks as if the mutations will not be more severe than the original, and the mutations will resemble the original closely enough for antibodies to effectively fight off these mutations.
Without a vaccine, how long will it take to develop herd immunity? Experts say that, in the absence of a vaccine, somewhere between forty and seventy percent of the world's population will likely become infected before herd immunity eventually eliminates the risk. World-wide that is somewhere between 3.1 and 5.5 billion people. On average about 3% of those infected are likely to die as a result –somewhere between 93 and 165 million people. (This number excludes the hundreds of millions who will die as a result of economic hardships brought about by lock-downs, other infectious diseases, extreme weather events like droughts and floods, locust plagues, etc.) The rest –somewhere between 3.0 and 5.3 billion people—will recover and develop immunity. The sooner all these people become infected and recover, the sooner we will develop global herd immunity. Once that happens the risk of COVID 19 epidemics will be all but entirely eliminated, (At least until our bodies stop producing antibodies or until a rogue mutant COVID 19 derivative virus manages to slip past the antibodies designed to fight off the original.)
But
how long is all this going to take? Weeks? Months? Years? The answer
to that question depends on a lot of variables. In wealthy countries
one variable is the ability or success of such countries in
'flattening the curve' –slowing the spread. The objective there is
minimizing the number of fatalities at the cost of delaying the
development of herd immunity (not to mention assuming unthinkable
amounts of public debt --a topic for another article). The flatter the curve, the longer it will take to achieve herd immunity. Because many wealthy countries like
Canada have an aging population, they are in some ways particularly vulnerable to COVID
19. But precisely because Canada does have a universal, albeit somewhat dilapidated
healthcare system, it can, at least to some degree, save many lives by bolstering the healthcare system in
response to this pandemic. Wealthy countries like Canada also have the economic resources to put a large proportion of their population in lock-down while still providing them with a livable income. In the national context, therefore, minimizing the
death toll by containing the spread seems to make a lot of sense for countries like Canada.
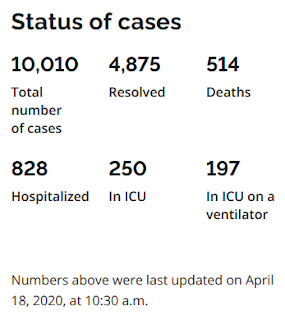 Herd Immunity in Canada: So
when will
Canada reach herd immunity? Its anybody's guess. But, despite the many variables, let's at least take a
stab at coming up with a somewhat educated guess. In Ontario, according to the
numbers in the adjacent table, we have about 10,000 known cases. The total population
of Ontario is around 14.4 million people. If we go with the lowest
number of infections required to reach herd immunity –40%-- we
will have to wait until another 5,760,000 citizens become infected and recover:
Herd Immunity in Canada: So
when will
Canada reach herd immunity? Its anybody's guess. But, despite the many variables, let's at least take a
stab at coming up with a somewhat educated guess. In Ontario, according to the
numbers in the adjacent table, we have about 10,000 known cases. The total population
of Ontario is around 14.4 million people. If we go with the lowest
number of infections required to reach herd immunity –40%-- we
will have to wait until another 5,760,000 citizens become infected and recover:
(40%
= 5,760,000 citizens required to reach herd immunity:
5,760,000 – 10,000 currently
confirmed as positive = 5,750,000 more to go)
(A chart also linked to on the WHO website, suggests that in Canada a minimum 56.5 % of the population will have to be infected before herd immunity is reached)
(A chart also linked to on the WHO website, suggests that in Canada a minimum 56.5 % of the population will have to be infected before herd immunity is reached)
Even
if there were actually already 500,000 mostly unconfirmed infections, at a rate of 500,000 infections per month it would still take at least a year to reach herd immunity in
Ontario.
Conclusion:
It
is difficult to come to any meaningful conclusions, given the fluidity
of the crisis, the great number of variables, the great number of
unknowns, and a great deal of conjecture. That said, I will
nevertheless assert the following:
In Canada:
- While the Provincial and Canadian governments may be able to pay non-essential workers to stay at home for a few more months, they cannot continue to do so indefinitely; there are not enough tools in the toolbox to support a lock-down for the number of years it will take before herd immunity is finally reached.
- Therefore the current lock-down will be lifted long before herd immunity is reached.
- Once those currently in lock-down resume circulation as part of their daily social and economic activities, the curve will begin to rise again --the rate of infection will again increase and continue to do so exponentially until social distancing is resumed.
- Healthcare facilities will be operating at full capacity, albeit at an increased capacity as scarce resources such as tests, ventilators, PPEs, etc become available, but may quickly become overwhelmed again as more and more after formerly locked down people begin to circulate and become infected and critically ill.
- With the increase in the rate of infection, herd immunity will be reached more quickly than it would have under a perfectly flat curve. How much more quickly depends on how great the increase in the rate of infection.
- Only the development and wide dissemination and administration of a safe and effective vaccine within a year or less would make reaching herd immunity possible in a timely manner.
Globally:
- The ability to protect themselves and their neighbours through self-isolation, social distancing, and accessing medical services is a privilege that most people on this planet don't enjoy. While the COVID 19 virus itself is not discriminatory --it just as happily infects wealthy people on cruise ships as those living in abject poverty in overcrowded slums or refugee camps-- the economic hardships incurred by vulnerable populations living in poor countries will be much greater. Those with few or no healthcare resources, or no ability to provide for the needs of citizens in a in lock-down situation, will suffer millions of deaths over and above those dying as a direct result of being infected by the virus itself.
- Countries in which the majority of the population lack the means for self-isolation and social distancing will reach herd immunity long before wealthier countries who do have the means and do practice social distancing.
There
are, of course, many more questions than answers that arise about the implications of this
pandemic. But trying answer them is beyond the scope of this
essay. Here are a few big questions for your consideration:
- What will be the long-term consequences of the public debt incurred by attempts to mitigate the worst effects of this virus? Who is going to pay that debt?
- Will the dominant global economic development model survive this pandemic? If not, what will replace it?
- Will there be a decrease in global inequality and a levelling of the playing field? Or will the pandemic increase global disparity?
- What is the primary objective of governments' unprecedented "quantitative easing" spending? Saving lives or saving the economy as we knew it?
- Will addressing the climate crisis become easier or more difficult as a result of this virus?
- What are the geopolitical implications of this virus? Will it result in a new balance of power globally?
- Will there be dramatic changes in the out-sourcing of manufactured goods?
- Will wealthy countries grant special privileges and employment opportunities to recovered COVID 19 victims for jobs in essential services? And/or rich countries import cheaper recovered workers for from poor countries? (grant them what is being referred to as an "immunity passport"? If so, how will this cause a brain-drain in poor countries as specialized workers in healthcare and other essential services take up more lucrative jobs in rich countries?
- What about the banks and financial institutions? Now that they are once again deregulated, will they extend credit to dubious businesses with few future prospects in a totally restructured global economy? Or will they choose to use the money to cancel the debts of clients the deem to be unlikely to succeed in a post-pandemic world? Are they laughing all the way to the bank? Are they poised to demand yet another bailout should their old and new clients prove unable to service existing debts?
- What will the long-term effect of unprecedented disaster capitalism --humongous corporate welfare checks and bail-outs, roll-back or elimination of environmental protection standards, resumption of arms sales to known human rights abusers, etc.-- be on the distribution of wealth and power in the post COVID 19 world? (See also this interview entitled "Coronavirus Is the Perfect Disaster for ‘Disaster Capitalism’" with Naomi Klein, author of "The Shock Doctrine" and Antony Loewenstein's "Disaster Capitalism: Making a Killing Out of Catastrophe".
- Which poses the greater existential threat to humanity: COVID 19? or the Climate Crisis?
These are but a few of the many questions for which I have no answers. Your thoughts?